How can we make public health more precise?
Highlights and videos from the Cambridge Public Health and Precision Health Initiative showcase
On Thursday 21 November 2024, Cambridge Public Health (CPH) Interdisciplinary Research Centre and Precision Health Strategic Research Initiative co-hosted a showcase exploring how precision medicine is reshaping public health.
The event explored the transformative potential of precision health, whilst also considering the challenges and risks that accompany these advancements.
The showcase was opened by Dr Nik Johnson, Mayor of Cambridgeshire and Peterborough Combined Authority
The showcase was opened by Dr Nik Johnson, Mayor of Cambridgeshire and Peterborough Combined Authority
The day opened with powerful remarks from Professor Aliko Ahmed, Regional Director of Public Health for East of England (NHS and OHID), and Dr Nik Johnson, Mayor of Cambridgeshire and Peterborough Combined Authority. Both speakers emphasised the profound impact of health inequalities on individuals, communities and society. While precision health holds great promise, it also raises a moral imperative: these innovations must work to reduce inequalities rather than reinforce them. This focus on health equity remained a central theme throughout the day.
Session 1
Early disease detection for patients, communities and populations
The first session explored approaches to early disease detection, illustrating the potential of precision health to address a range of health conditions. Professor Nora Pashayan shared her work on Precision Cancer screening, advocating for a risk-stratified approach tailored to individual health profiles. Dr Coco Newton discussed developments in cognitive assessment for early dementia screening and the potential of tools such as wearables and blood tests to identify early signs of the disease. Finally, Dr Anna Moore focused on child mental health, emphasising the urgent need for timely identification and prevention of child mental health problems.

Session 2
Precision public health
The second session explored how new technologies, in both wearables and in social media, can inform health by providing novel methods of data collection and analysis. Dr Kirsten Rennie discussed the use of wearables to remotely collect patient data and the practical considerations for using these devices in health care. Dr Amy Orben introduced the concept of data donation, and the potential of analysing social media data for deeper insights relating to children’s mental health.
Dr Amy Orben spoke about data donation to support research about chilren's mental health
Dr Amy Orben spoke about data donation to support research about chilren's mental health
Ron Zimmern, founder of the Public Health Genomics Foundation, closed the session by reflecting on his career in genomics and public health. He critiqued the limitations of a “one-size-fits-all” approach to public health, championing a move towards a more personalised approach to health care.
Session 3
Inclusive health and care systems
The third session opened with Dr Adewunmi Akingbola, winner of the CPH Early Career Researcher competition, presenting his work on methods to estimate Hepatitis C prevalence among people who inject drugs in the UK. Find out more about Dr Akingbola in our latest Researcher spotlight.
Dr Adewunmi Akingbola, winner of the Early Career Researcher competition
Dr Adewunmi Akingbola, winner of the Early Career Researcher competition
Professor David Rowitch and Dr Ian Hosking then shared insights on fostering inclusivity in hospital design, using Cambridge Children’s Hospital as a case study. Dr Hosking introduced a pioneering tool designed to identify visual stress in buildings, allowing architectural design to create more supportive health care environments and reducing the risk of seizures.
Dr Rosalind Parkes-Ratanshi closed the session with a global perspective on precision public health. She explored the opportunities and challenges of precision public health in low- and middle-income countries, providing examples from her work on HIV in Uganda including delivering Antiretrovirals by drones.
Session 4
The future of Precision Public Health
The final session focused on what the future might hold for precision public health, blending historical perspectives, technological innovation, and community engagement. Dr Philippa Carter provided a historical lens with a case study of Gheel, Belgium—a centuries-old model of community-based mental health care that continues to inspire care approaches today.
Dr Gemma Bale followed with an engaging presentation on new wearable technology using near-infrared spectroscopy to measure brain activity. By detecting oxygenation levels in real time, this innovation offers new possibilities for monitoring brain function.
Professor Leslie Leve from the University of Oregon spoke about the role of community engagement approaches in research to drive equitable precision health.
The conference concluded with a keynote speech from Professor Frank Kee from Queen’s University Belfast, who shared his vision of how we can make public health more precise. He explored both philosophical and practical considerations, questioning whether precision medicine is the right paradigm for improving population health. By seeking common ground between precision health and public health, he urged caution and care in charting the path forward.

Audience perspectives
Opportunities and challenges in making public health more precise
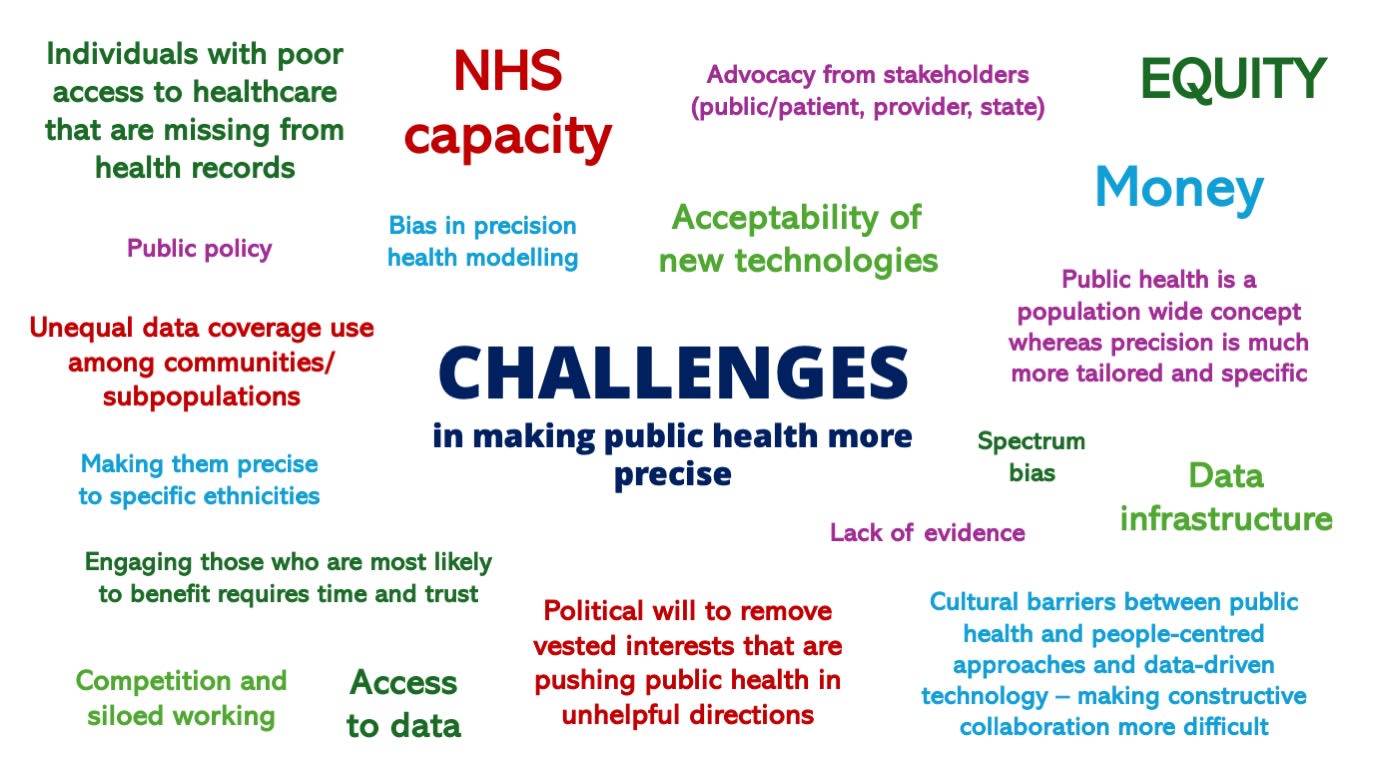
As part of the showcase, participants were asked to share their perspectives on the opportunities and challenges in advancing precision public health. The responses highlighted a rich diversity of ideas and concerns.
On the opportunities side, key themes included the use of advanced technologies like wearables and biosensors, and the ability to leverage large datasets to inform targeted interventions. Participants also emphasised the importance of enabling equitable access to health care and the role of risk-stratified screening.
Conversely, the challenges identified were also compelling. Issues such as unequal data representation, NHS capacity constraints, and the risk of reinforcing health inequalities emerged as significant barriers. Participants also pointed to the complexities of integrating new technologies into existing systems, ensuring the cultural acceptability of innovations, and addressing political and structural hurdles, such as data infrastructure and vested interests.
The showcase brought together and highlighted the exciting research taking place across Cambridge University from a range of disciplines, offering fresh perspectives on how precision health is shaping the future of public health. From early disease detection to global health equity, the event underscored both the promise and the responsibility of advancements in precision health. The discussions encouraged consideration of how innovation can be harnessed to advance equity and contribute to a healthier, more inclusive future.
Early Career Researcher
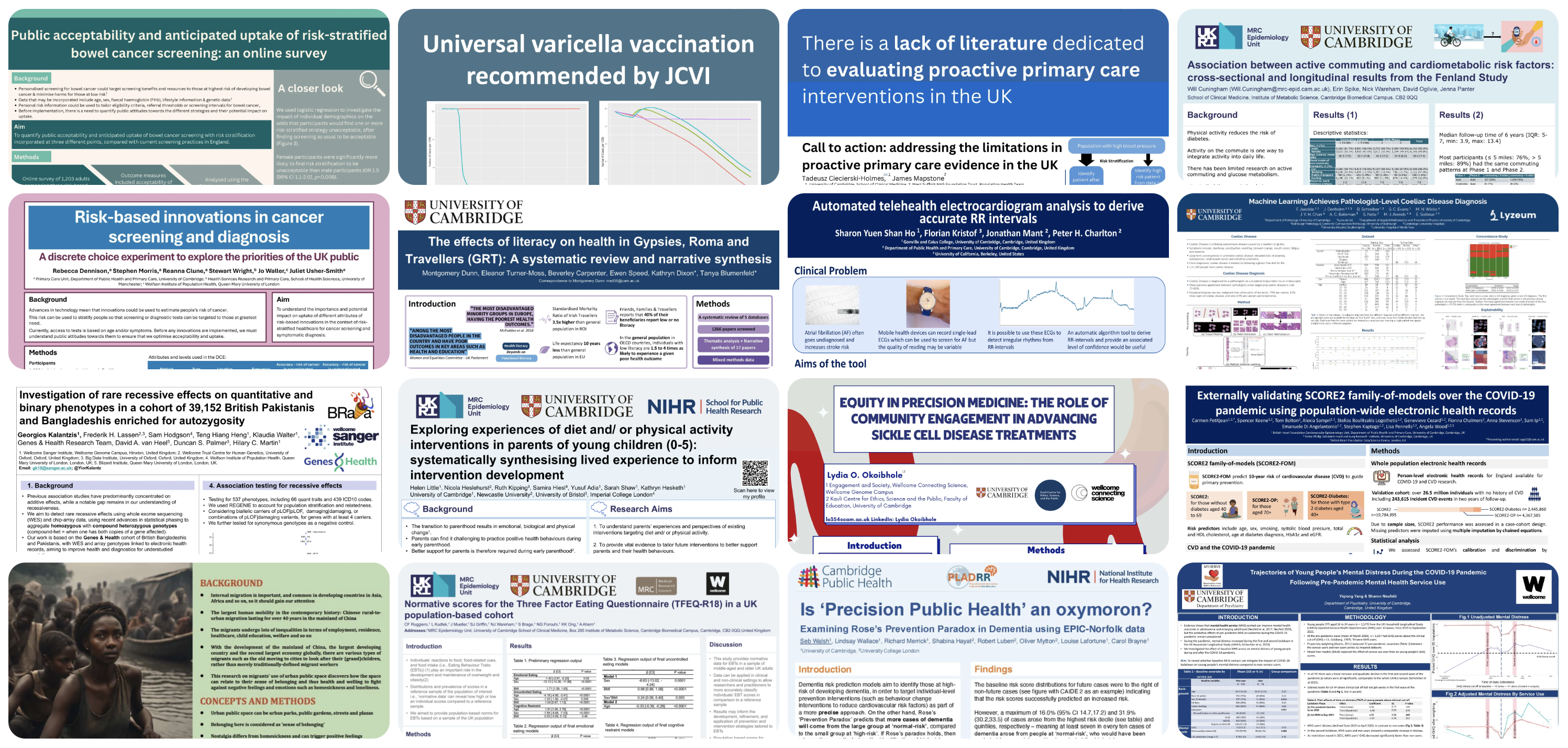
Poster Gallery

Attendees of the showcase were treated to a gallery of creative and thought-provoking posters designed by early career researchers as part of a poster competition that attracted submissions from across the university. The winner was Lily Taylor's poster on Public acceptability and anticipated uptake of risk-stratified bowel cancer screening, was awarded first place by the panel of judges.
Click on the image below to view all the posters gallery